Know more
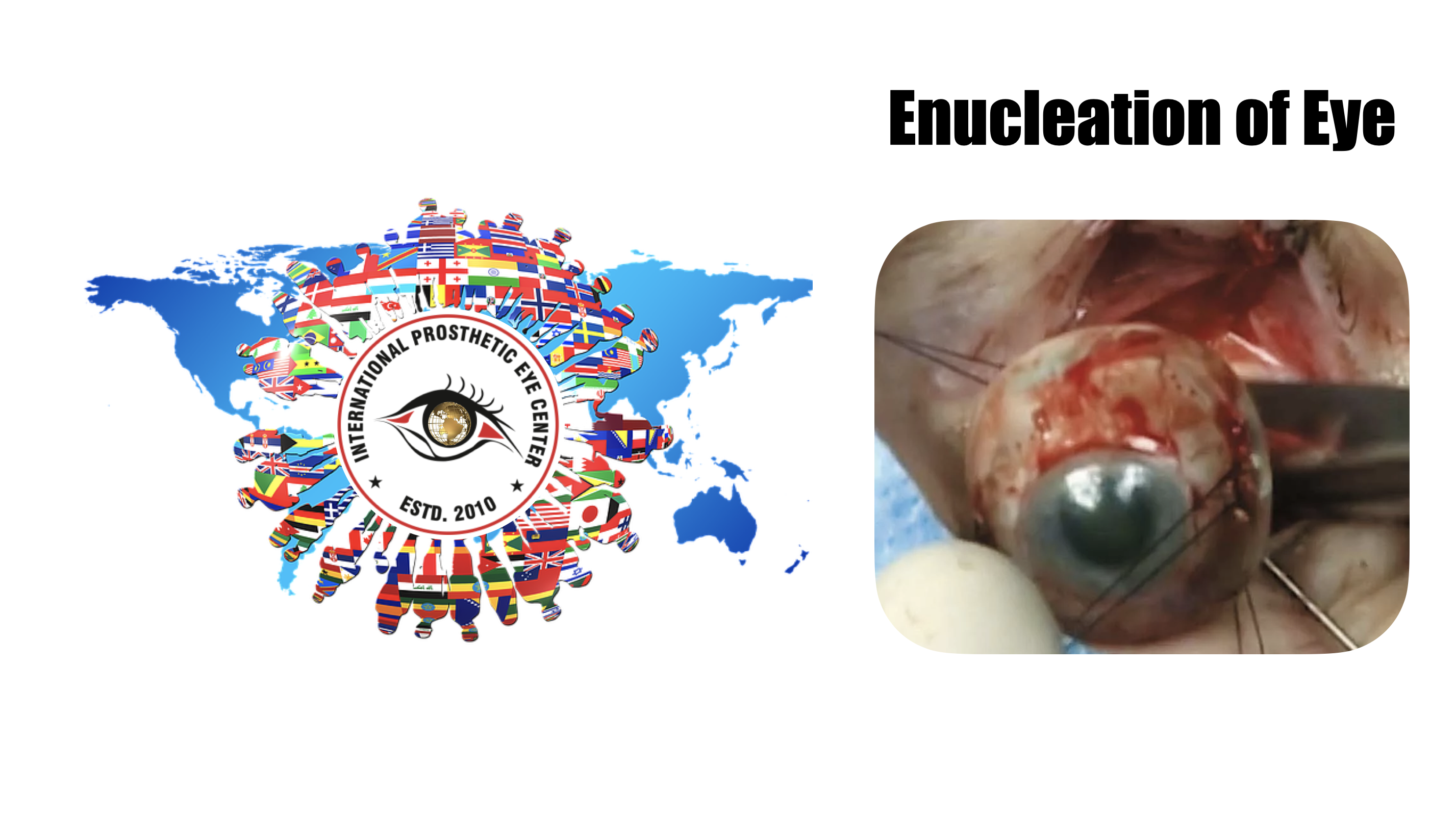
enucleation of the Eye
Enucleation is the surgical procedure that involves removal of the entire globe and its intraocular contents, with preservation of all other periorbital and orbital structures. Enucleation is in contrast to evisceration, in which the ocular contents are removed from an intact sclera, and exenteration, in which the entire orbital contents, including the globe and soft tissues, are removed.
Background
The surgical removal of the eye was first reported in the 1500s as a procedure known as extirpation.[1] Unlike an enucleation, the conjunctiva and extraocular muscles were not spared. By the mid 1800s, an enucleation without implant placement was described in the literature. The first reports of implant insertion following enucleation were described in 1886 and 1887, with variable success in implant retention.[1]
Indications
The following are indications for enucleation:
Intraocular malignancy or high suspicion for intraocular malignancy (most commonly uveal melanoma and retinoblastoma)
Trauma without visual potential
Blind, painful eye
Severe infection without visual potential
Sympathetic ophthalmia
Microphthalmos
The role of primary enucleation in acute trauma remains controversial, particularly when a patient's mental status may be altered and/or they are unable to consent. Many surgeons advocate for primary closure of an open globe with later consideration for an enucleation if the eye remains no light perception or becomes painful without vision. Enucleation of an eye can be associated with significant psychological trauma, and the approach of primary globe repair provides the patient to consider their options and the pros and cons of enucleation after the initial trauma and any altered mental status has resolved and provides autonomy to elect this operation in the future. The rare risk of sympathetic ophthalmia in the uninvolved eye must be considered and discussed with the patient. In select cases where the eye is determined to have no visual potential, when repair or at least primary closure of the globe is determined to be impossible, and/or the medical comorbidities of the patient are significant, the surgeon may elect to perform primary enucleation.
Advantages
In contrast to evisceration, enucleation allows for histologic examination of an intact globe and optic nerve. This is particularly important in settings of biopsy-proven or suspected intraocular malignancy, in which it is essential to determine the margins of the malignancy and invasion of the optic nerve, if any.
When comparing the aesthetics of an enucleated socket to an eviscerated socket, one retrospective study showed no statistically significant difference between enucleation and evisceration patients graded by both patients and masked observers.[2]
Enucleation classically has been thought to decrease the risk of sympathetic ophthalmia as it avoids exposure to uveal antigens that may occur during an evisceration.[3] However, more recent studies have reported no cases of sympathetic ophthalmia following evisceration.[4][5]
Disadvantages
A reduction in implant motility is often noted in enucleations. Compared to patients who underwent evisceration, one study found enucleation patients to have statistically significant poorer implant motility.[2] However, no difference in prosthesis motility was noted between evisceration and enucleation patients.
In a 2003 survey of all board-certified ocularists in the United States, 92% reported preferring evisceration to enucleation for a patient who required removal of the eye.[6] Eighty-two percent of survey respondents believed that evisceration afforded the best ocular motility and best overall cosmetic outcome, and 94% percent believed that complications of enophthalmos and/or deep superior sulcus were more common after enucleations.
Surgical Technique
An enucleation is often performed as an outpatient procedure under general anesthesia. A retrobulbar block of local anesthetic with epinephrine is administered to aid in hemostasis and postoperative pain management. After a time-out is performed to confirm the correct operative eye with the entire operating room team, the face is prepared and draped in sterile fashion. A limbal conjunctival peritomy is performed with Wescott scissors for 360 degrees. Blunt dissection in the sub-Tenon's plane is then carried out in each of the oblique quadrants. Each rectus muscle is then identified, isolated with a muscle hook, secured with suture, and cut at the insertion to the globe. The superior and inferior oblique muscles are isolated and generally transected, though some surgeons prefer to tag these as well. Conversely, some surgeons prefer to secure the muscles with suture after the eye has been removed.[7]
Once the globe is determined to rotate freely, the optic nerve is identified, strummed, and cut with enucleation scissors or an enucleation snare wire. Some surgeons prefer to first clamp the optic nerve with a curved hemostat prior to transection to encourage further hemostasis. An attempt should be made to cut a long segment of the optic nerve, particularly in situations of intraocular malignancy where histologic examination of the optic nerve is crucial. Additional hemostasis is then achieved with direct pressure in the intraconal space and cautery of the optic nerve if needed.
An implant is then placed in the intraconal space to replace volume lost by the enucleated globe, achieve cosmetic symmetry with the fellow socket, and allow for motility of the prosthesis. To determine appropriate diameter of the implant, use of the formula axial length-2 mm has been shown to provide for adequate replacement of lost volume and minimize superior sulcus deformity and enophthalmos.[8] A sizing set can also be used to determine the appropriate size intraoperatively.
In certain circumstances including severe infection, a surgeon may choose not to place an implant at the time of enucleation and elect to place an implant in a second surgery. The extraocular muscles are generally attached to each other anterior to the implant or sutured directly to a porus or wrapped implant. A two-layered closure is then carried out with absorbable sutures, first of Tenon’s capsule and then of the conjunctiva. Antibiotic ointment is applied, a clear plastic conformer is placed over the closed conjunctiva, and a pressure patch is placed over the socket. A temporary tarsorrhaphy may be placed.