KNOW MORE ABOUT
MICROTIA
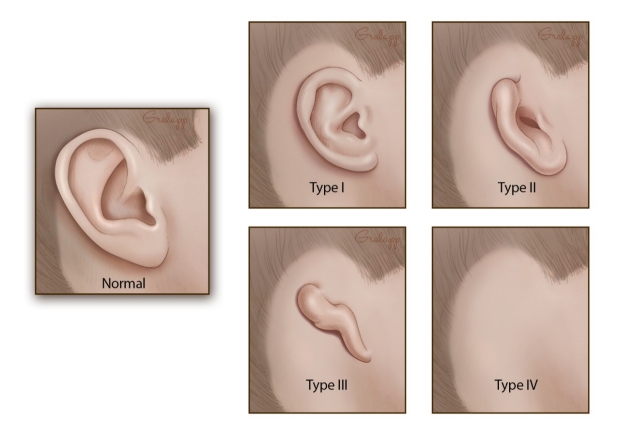
Microtia is a congenital deformity where the pinna (external ear) is underdeveloped. A completely undeveloped pinna is referred to as anotia. Because microtia and anotia have the same origin, it can be referred to as microtia-anotia. Microtia can be unilateral (one side only) or bilateral (affecting both sides).
Treatment
The goal of medical intervention is to provide the best form and function to the underdeveloped ear.
Hearing
Typically, testing is first done to determine the quality of hearing. This can be done as early as in the first two weeks with a BAER test (Brain Stem Auditory Response Test). At age 5–6, CT or CAT scans of the middle ear can be done to elucidate its development and clarify which patients are appropriate candidates for surgery to improve hearing. For younger individuals, this is done under sedation.
The hearing loss associated with congenital aural atresia is a conductive hearing loss—hearing loss caused by inefficient conduction of sound to the inner ear. Essentially, children with aural atresia have hearing loss because the sound cannot travel into the (usually) healthy inner ear—there is no ear canal, no eardrum, and the small ear bones (malleus/hammer, incus/anvil, and stapes/stirrup) are underdeveloped. "Usually" is in parentheses because rarely, a child with atresia also has a malformation of the inner ear leading to a sensorineural hearing loss (as many as 19% in one study).Sensorineural hearing loss is caused by a problem in the inner ear, the cochlea. Sensorineural hearing loss is not correctable by surgery, but properly fitted and adjusted hearing amplification (hearing aids) generally provide excellent rehabilitation for this hearing loss. If the hearing loss is severe to profound in both ears, the child may be a candidate for a cochlear implant (beyond the scope of this discussion).
Unilateral sensorineural hearing loss was not generally considered a serious disability by the medical establishment before the nineties; it was thought that the afflicted person was able to adjust to it from birth. In general, there are exceptional advantages to gain from an intervention to enable hearing in the microtic ear, especially in bilateral microtia. Children with untreated unilateral sensorineural hearing loss are more likely to have to repeat a grade in school and/or need supplemental services (e.g., FM system – see below) than their peers.
Children with unilateral sensorineural hearing loss often require years of speech therapy in order to learn how to enunciate and understand spoken language. What is truly unclear, and the subject of an ongoing research study, is the effect of unilateral conductive hearing loss (in children with unilateral aural atresia) on scholastic performance. If atresia surgery or some form of amplification is not used, special steps should be taken to ensure that the child is accessing and understanding all of the verbal information presented in school settings. Recommendations for improving a child's hearing in the academic setting include preferential seating in class, an FM system (the teacher wears a microphone, and the sound is transmitted to a speaker at the child's desk or to an ear bud or hearing aid the child wears), a bone-anchored hearing aid (BAHA), or conventional hearing aids. Age for BAHA implantation depends on whether the child is in Europe (18 months) or the US (age 5). Until then it is possible to fit a BAHA on a softband
It is important to note that not all children with aural atresia are candidates for atresia repair. Candidacy for atresia surgery is based on the hearing test (audiogram) and CT scan imaging. If a canal is built where one does not exist, minor complications can arise from the body's natural tendency to heal an open wound closed. Repairing aural atresia is a very detailed and complicated surgical procedure which requires an expert in atresia repair. While complications from this surgery can arise, the risk of complications is greatly reduced when using a highly experienced otologist. Atresia patients who opt for surgery will temporarily have the canal packed with gelatin sponge and silicone sheeting to prevent closure. The timing of ear canal reconstruction (canalplasty) depends on the type of external ear (Microtia) repair desired by the patient and family. Two surgical teams in the USA are currently able to reconstruct the canal at the same time as the external ear in a single surgical stage (one stage ear reconstruction).
In cases where a later surgical reconstruction of the external ear of the child might be possible, positioning of the BAHA implant is critical. It may be necessary to position the implant further back than usual to enable successful reconstructive surgery – but not so far as to compromise hearing performance. If the reconstruction is ultimately successful, it is easy to remove the percutaneous BAHA abutment. If the surgery is unsuccessful, the abutment can be replaced and the implant re-activated to restore hearing.
External ear
The age when outer ear surgery can be attempted depends upon the technique chosen. The earliest is 7 for Rib Cartilage Grafts. However, some surgeons recommend waiting until a later age, such as 8–10 when the ear is closer to adult size. External ear prostheses have been made for children as young as 5.
For auricular reconstruction, there are several different options:
Ear Prosthesis: An auricular (ear) prosthesis is custom made by an anaplastologist to mirror the other ear. Prosthetic ears can appear very realistic. They require a few minutes of daily care. They are typically made of silicone, which is colored to match the surrounding skin and can be attached using either adhesive or with titanium screws inserted into the skull to which the prosthetic is attached with a magnetic or bar/clip type system. These screws are the same as the BAHA (bone anchored hearing aid) screws and can be placed simultaneously. The biggest advantage over any surgery is having a prosthetic ear that allows the affected ear to appear as normal as possible to the natural ear.
Rib Cartilage Graft Reconstruction: This surgery may be performed by specialists in the technique. It involves sculpting the patient's own rib cartilage into the form of an ear. Because the cartilage is the patient's own living tissue, the reconstructed ear continues to grow as the child does. In order to be sure that the rib cage is large enough to provide the necessary donor tissue, some surgeons wait until the patient is 8 years of age;however, some surgeons with more experience with this technique may begin the surgery on a child aged six The major advantage of this surgery is that the patient's own tissue is used for the reconstruction. This surgery varies from two to four stages depending on the surgeon's preferred method. A novel one stage ear reconstruction technique is performed by a few select surgeons. One team is able to reconstruct the entire external ear and ear canal in one operation.
Reconstruct the ear using a polyethylene plastic implant (also called Medpor): This is a 1–2 stage surgery that can start at age 3 and can be done as an outpatient without hospitalization. Using the porous framework, which allows the patient's tissue to grow into the material and the patient's own tissue flap, a new ear is constructed in a single surgery. A small second surgery is performed in 3–6 months if needed for minor adjustments. Medpor was developed by John Reinisch. This surgery should only be performed by experts in the techniques involved. The use of porous polyethylene implants for ear reconstruction was initiated in the 1980s by Alexander Berghaus.